Blog

Why are Sepsis and Staph Infections So Common in Hospitals?
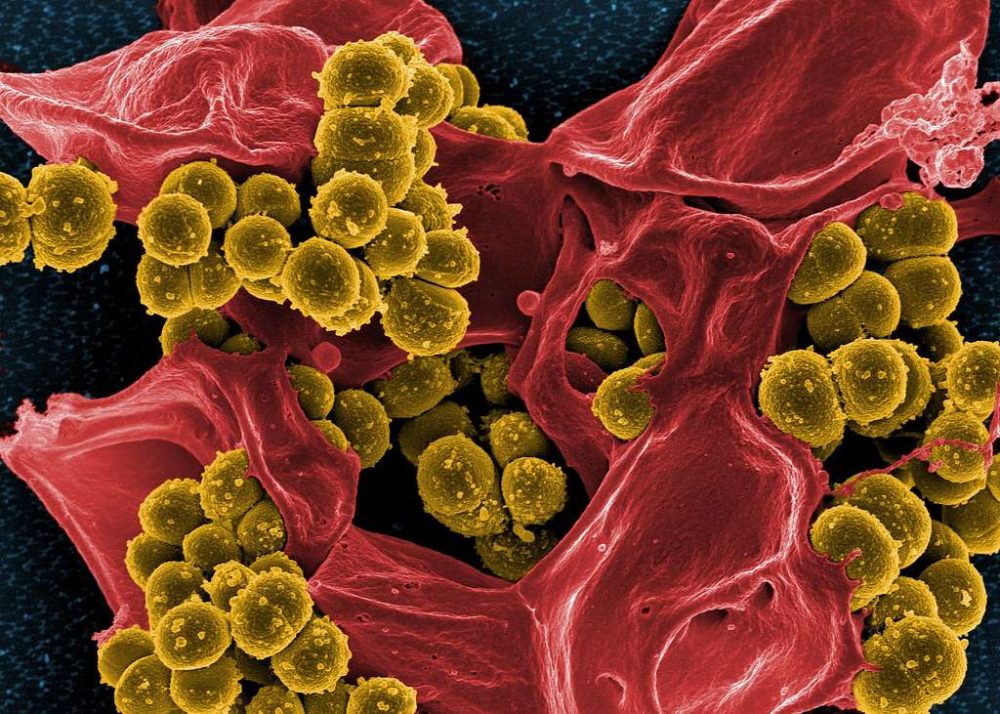
Each year, 1.7 million adults in the United States are diagnosed with sepsis, a severe and potentially fatal blood infection. Since healthcare facilities are supposed to be clean and safe places where you go to get better, it might surprise you to learn that so many people get staph infections and sepsis while they’re in the hospital being treated for something else.
In honor of Patient Safety Awareness Week, we’re here to explain what causes these infections and how healthcare professionals like Sterile Processing Technicians (CSPTs) help prevent them.
What Are Staph Infections and Sepsis?
Sepsis is when an infection in the body has spread into the bloodstream. The reason it is so dangerous is because sepsis causes collateral damage to vital organs. This damage can lead to further health issues and potentially death.
Staphylococcus aureus, or “Staph,” is a type of germ often found on human skin and on surfaces and objects that touch the skin. While the germ does not always harm people, it can get into the bloodstream and cause sepsis or even death. This infection often spreads through cuts, abrasions, and occasionally skin-to-skin contact.
Although most sepsis cases originate outside the hospital, around 15% are contracted within hospital settings. One study showed that sepsis contributes to between a third to a half of all U.S. hospital deaths. That’s more common than heart attack and stroke combined.
Why Are Infections Common in Hospitals and Medical Facilities?
In healthcare facilities, the risk of more serious staph infection is higher for 3 main reasons:
(1) Healthcare facilities are where people go when they’re sick, so the buildings will inevitably have an array of bacteria and other pathogens in the air and on surfaces. This also includes medical professionals. If a doctor or nurse does not wash their hands or wear gloves before examining your incisions or surgery, they may transfer bacteria into your wound.
(2) A primary infection risk factor is invasive procedures like surgery. The insertion of catheters and the use of ventilators are also risk factors for developing sepsis. These procedures can introduce bacteria or other pathogens into the body. Post-surgery staph infection can also arise due to dirty linen or contaminated surgical equipment.
(3) While anyone can develop sepsis, immunocompromised patients are the most at risk. This includes people with diabetes, babies, older adults, and cancer patients. In healthcare facilities, it is natural that many patients have weakened immune systems, especially after undergoing a procedure. A urinary tract infection or cold could open the door to further infection in immune-suppressed people.
How Do Hospitals Prevent Sepsis and Other Infections?
Since sepsis is relatively common and has the potential to be life-threatening, hospitals have strict protocols and standards. Measures to prevent infection involve strict cleaning routines and sterilizing areas and tools used in patient care.
This sterilization is done by Central Service Processing Technicians or CSPTs. A CSPT is responsible for ensuring that all medical instruments are clean and safe for the patient. They are the first line of defense against infection in a hospital. CSPTs ensure that all equipment is safe before encountering a doctor.
From here, hospitals often have processes in place to prevent infection by keeping sterile environments, mandating patient care regulations, and more.
The Role of CPSTs in Preventing Hospital Infections
A CSPT is among the most critical lines of defense against sepsis or staph infections. Their work allows doctors and medical professionals to know that any medical equipment is clean and properly prepared before reaching the patient. This keeps operating rooms free from infection, allows emergency procedures to run with a lowered risk of contamination, and keeps patients focused on their healthcare goals and not on risks.
Start Your Career in Infection Prevention Today!
Hospital-acquired infections like sepsis and staph are serious health risks, but CSPTs are critical in keeping patients safe. If you’re passionate about healthcare and want to make a real impact, a career in sterile processing could be for you.
At Swedish Institute, our CSPT training program provides the skills and hands-on experience you need to become a key player in hospital infection control. Train with industry experts, gain valuable certification, and step into a rewarding career in healthcare.
- Learn proper sterilization techniques
- Prepare for a career in hospitals, surgical centers, and more
- Help protect patients from life-threatening infections
Take the first step today! Contact Swedish Institute to learn more about our CSPT training program. Start your journey toward a career in healthcare safety.
Apply Now! Or call us at (866) 673-6148to get started!
FAQs
1. What are the leading causes of hospital-acquired infections?
Hospital-acquired infections (HAIs) occur when bacteria, viruses, or fungi enter the body through contaminated medical equipment, unwashed hands, or open wounds. Patients undergoing surgery, catheter insertions, or ventilator use are at higher risk due to exposure to germs in a sterile environment.
2. What are the best hospital infection control measures?
Hospitals follow strict infection control protocols, including hand hygiene, sterilization of medical tools, use of personal protective equipment (PPE), and patient monitoring. These measures help reduce the risk of infections like sepsis and staph.
3. Why are staph infections and sepsis common in hospitals?
Hospitals care for sick patients, many of whom have weakened immune systems. Invasive procedures (such as surgeries, IV lines, and catheters) increase infection risk. Staphylococcus bacteria are also commonly found on skin and surfaces, making them easy to spread.
4. How do hospitals prevent infections like sepsis?
Hospitals use strict infection control measures, including:
- Sterilizing medical instruments and surfaces
- Enforcing hand hygiene protocols for staff and visitors
- Using personal protective equipment (PPE) like gloves and masks
- Following strict surgical site care guidelines to prevent contamination
5. What are the symptoms of a hospital-acquired infection?
Symptoms vary depending on the type of infection but may include:
- Fever and chills
- Redness, swelling, or pus at a surgical site
- Difficulty breathing (for pneumonia-related infections)
- Unusual pain or fatigue
- Confusion or dizziness (a sign of sepsis)
6. How can patients reduce their risk of infection in hospitals?
Patients can take these steps to lower their risk:
- Ask doctors and nurses to wash their hands before examining you.
- Keep surgical wounds clean and dry as directed.
- Speak up if catheters, IVs, or bandages seem dirty or have been left in too long.
- Follow post-surgery care instructions closely.
- Maintain good personal hygiene and avoid unnecessary contact with other patients.
7. Who is most at risk for hospital-acquired infections?
Patients with a weakened immune system are at higher risk, including:
- Older adults
- Newborns and infants
- Cancer patients undergoing chemotherapy
- Diabetics and people with chronic illnesses
- Patients with catheters, breathing tubes, or surgical wounds
8. How do CSPTs help prevent infections in hospitals?CSPTs are critical in infection prevention by sterilizing surgical tools, disinfecting hospital equipment, and ensuring that medical instruments are adequately prepared before use. Their work minimizes contamination risks in operating rooms and patient care areas.
Recent Posts
- An Inside Look at Medical Assistant Classes
- Why are Sepsis and Staph Infections So Common in Hospitals?
- Mental Health, Nursing, and Education: Meet Swedish Institute Grad Omarr Savage
- From Student to Employer: Two Swedish Institute Grads Tell Their Success Stories
- Going Back to College After Time in the Workforce: A How-To Guide